Personalized gene editing saved one baby — could it be expanded to many?
Rokna Social Desk: gene therapy, CRISPR, base editing, personalized medicine, rare diseases, genetic research, biotechnology, medical innovation, precision medicine, clinical trials, genetic disorders, pediatric medicine
According to Rokna, citing the Nature news, late last year, dozens of scientists spread across continents joined forces in a race against time to save the life of a baby boy. The result was unprecedented: a pioneering gene-editing therapy created specifically for a single individual, completed in a record six months.
Now, baby KJ Muldoon’s medical team is preparing to repeat that achievement — not just once, but at least five more times, and even faster.
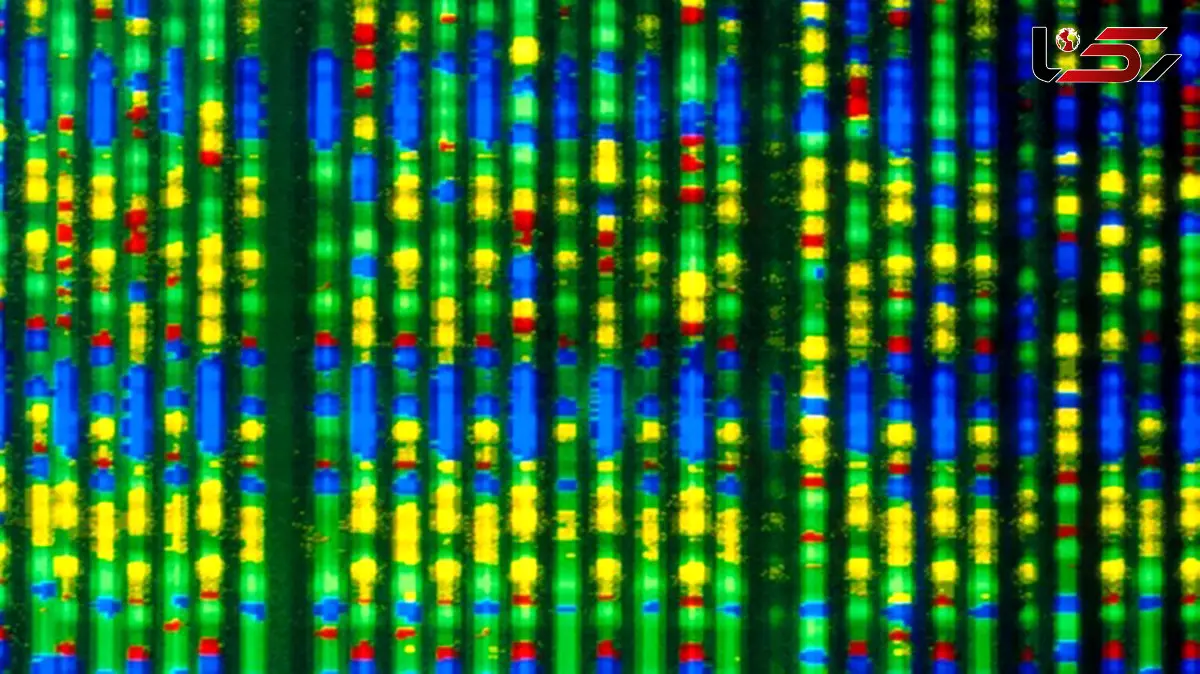
The landmark clinical trial, described on 31 October in the American Journal of Human Genetics, will utilize a variation of the CRISPR–Cas9 gene-editing technology known as base editing, which enables researchers to make precise, one-letter modifications to DNA sequences. The study is expected to launch next year, following months of negotiations with US regulators aimed at streamlining the complex approval process that typically precedes human trials for such treatments.
“It was a pretty hectic and intense six months,” said Kiran Musunuru, a cardiologist at the Perelman School of Medicine at the University of Pennsylvania and one of KJ’s treating physicians. “But I believe we can shorten it further.”

The upcoming trial marks the next step toward addressing a question that has resonated among many families of children suffering from rare genetic disorders since the success of KJ’s treatment: when will it be our turn?
“There is no single model that fits everyone in this field,” said Ryan Maple, executive director of the Global Foundation for Peroxisomal Disorders in Tulsa, Oklahoma.
Momentum appears to be gathering. Beyond the planned trial in Philadelphia, the Center for Pediatric CRISPR Cures, launched in July by the University of California, Berkeley, and the University of California, San Francisco, also aims to create customized gene-editing therapies. Meanwhile, in September, the US government’s Advanced Research Projects Agency for Health (ARPA-H) unveiled two new initiatives to fund research into developing and manufacturing “precision genetic medicines.”
“I’m more optimistic now than I’ve ever been,” said Joseph Hacia, a medical geneticist at the Keck School of Medicine at the University of Southern California in Los Angeles.
A therapy for one
In August of last year, shortly after KJ Muldoon’s birth, doctors discovered that he carried a rare genetic mutation that prevented his body from producing a normal version of a vital liver enzyme called carbamoyl phosphate synthetase 1 (CPS1). This enzyme detoxifies ammonia — a waste product formed as the body breaks down proteins. When ammonia accumulates in the blood, it can cause severe brain damage, and most infants with CPS1 deficiency do not survive long enough to undergo the only available cure: a liver transplant.
But one of KJ’s doctors, Rebecca Ahrens-Nicklas of the Children’s Hospital of Philadelphia, had been collaborating with Musunuru to design a base-editing therapy that could be deployed rapidly for children with metabolic disorders. KJ would become their first patient.
In late February, he received a gene-editing therapy tailored uniquely to his DNA. CPS1 deficiency affects roughly one in a million births, and the therapy was engineered to locate one incorrect letter in his CPS1 gene sequence and replace it with the correct one, restoring the production of the full CPS1 enzyme.
After treatment, KJ’s ammonia levels fell significantly, and his need for medication decreased. Since then, he has made steady progress — learning to stand, eat solid food, and take his first steps.
“We celebrate every milestone KJ achieves,” said his mother, Nicole Aaron. “He has a light within him that brightens every room he enters.”
Send Comments